- Home
- Quintessential Queensland
- Distinctiveness
- Perceptions
- Perceptions: how people understand the landscape
- From runs to closer settlement
- Geological survey of Queensland
- Mapping a new colony, 1860-80
- Mapping the Torres Strait: from TI to Magani Malu and Zenadh Kes
- Order in Paradise: a colonial gold field
- Queensland atlas, 1865
- Queensland mapping since 1900
- Queensland: the slogan state
- Rainforests of North Queensland
- Walkabout
- Queenslanders
- Queenslanders: people in the landscape
- Aboriginal heroes: episodes in the colonial landscape
- Australian South Sea Islanders
- Cane fields and solidarity in the multiethnic north
- Chinatowns
- Colonial immigration to Queensland
- Greek Cafés in the landscape of Queensland
- Hispanics and human rights in Queensland’s public spaces
- Italians in north Queensland
- Lebanese in rural Queensland
- Queensland clothing
- Queensland for ‘the best kind of population, primary producers’
- Too remote, too primitive and too expensive: Scandinavian settlers in colonial Queensland
- Distance
- Movement
- Movement: how people move through the landscape
- Air travel in Queensland
- Bicycling through Brisbane, 1896
- Cobb & Co
- Journey to Hayman Island, 1938
- Law and story-strings
- Mobile kids: children’s explorations of Cherbourg
- Movable heritage of North Queensland
- Passages to India: military linkages with Queensland
- The Queen in Queensland, 1954
- Transient Chinese in colonial Queensland
- Travelling times by rail
- Pathways
- Pathways: how things move through the landscape and where they are made
- Aboriginal dreaming paths and trading ways
- Chinese traders in the nineteenth century
- Introducing the cane toad
- Pituri bag
- Press and the media
- Radio in Queensland
- Red Cross Society and World War I in Queensland
- The telephone in Queensland
- Where did the trams go?
- ‘A little bit of love for me and a murder for my old man’: the Queensland Bush Book Club
- Movement
- Division
- Separation
- Separation: divisions in the landscape
- Asylums in the landscape
- Brisbane River
- Changing landscape of radicalism
- Civil government boundaries
- Convict Brisbane
- Dividing Queensland - Pauline Hanson’s One Nation Party
- High water mark: the shifting electoral landscape 2001-12
- Hospitals in the landscape
- Indigenous health
- Palm Island
- Secession movements
- Separate spheres: gender and dress codes
- Separating land, separating culture
- Stone walls do a prison make: law on the landscape
- The 1967 Referendum – the State comes together?
- Utopian communities
- Whiteness in the tropics
- Conflict
- Conflict: how people contest the landscape
- A tale of two elections – One Nation and political protest
- Battle of Brisbane – Australian masculinity under threat
- Dangerous spaces - youth politics in Brisbane, 1960s-70s
- Fortress Queensland 1942-45
- Grassy hills: colonial defence and coastal forts
- Great Shearers’ Strike of 1891
- Iwasaki project
- Johannes Bjelke-Petersen: straddling a barbed wire fence
- Mount Etna: Queensland's longest environmental conflict
- Native Police
- Skyrail Cairns (Research notes)
- Staunch but conservative – the trade union movement in Rockhampton
- The Chinese question
- Thomas Wentworth Wills and Cullin-la-ringo Station
- Separation
- Dreaming
- Imagination
- Imagination: how people have imagined Queensland
- Brisbane River and Moreton Bay: Thomas Welsby
- Changing views of the Glasshouse Mountains
- Imagining Queensland in film and television production
- Jacaranda
- Literary mapping of Brisbane in the 1990s
- Looking at Mount Coot-tha
- Mapping the Macqueen farm
- Mapping the mythic: Hugh Sawrey's ‘outback’
- People’s Republic of Woodford
- Poinsettia city: Brisbane’s flower
- The Pineapple Girl
- The writers of Tamborine Mountain
- Vance and Nettie Palmer
- Memory
- Memory: how people remember the landscape
- Anna Wickham: the memory of a moment
- Berajondo and Mill Point: remembering place and landscape
- Cemeteries in the landscape
- Landscapes of memory: Tjapukai Dance Theatre and Laura Festival
- Monuments and memory: T.J. Byrnes and T.J. Ryan
- Out where the dead towns lie
- Queensland in miniature: the Brisbane Exhibition
- Roadside ++++ memorials
- Shipwrecks as graves
- The Dame in the tropics: Nellie Melba
- Tinnenburra
- Vanished heritage
- War memorials
- Curiosity
- Curiosity: knowledge through the landscape
- A playground for science: Great Barrier Reef
- Duboisia hopwoodii: a colonial curiosity
- Great Artesian Basin: water from deeper down
- In search of Landsborough
- James Cook’s hundred days in Queensland
- Mutual curiosity – Aboriginal people and explorers
- Queensland Acclimatisation Society
- Queensland’s own sea monster: a curious tale of loss and regret
- St Lucia: degrees of landscape
- Townsville’s Mount St John Zoo
- Imagination
- Development
- Exploitation
- Transformation
- Transformation: how the landscape has changed and been modified
- Cultivation
- Empire and agribusiness: the Australian Mercantile Land and Finance Company
- Gold
- Kill, cure, or strangle: Atherton Tablelands
- National parks in Queensland
- Pastoralism 1860s–1915
- Prickly pear
- Repurchasing estates: the transformation of Durundur
- Soil
- Sugar
- Sunshine Coast
- The Brigalow
- Walter Reid Cultural Centre, Rockhampton: back again
- Survival
- Survival: how the landscape impacts on people
- Brisbane floods: 1893 to the summer of sorrow
- City of the Damned: how the media embraced the Brisbane floods
- Depression era
- Did Clem Jones save Brisbane from flood?
- Droughts and floods and rail
- Missions and reserves
- Queensland British Food Corporation
- Rockhampton’s great flood of 1918
- Station homesteads
- Tropical cyclones
- Wreck of the Quetta
- Pleasure
- Pleasure: how people enjoy the landscape
- Bushwalking in Queensland
- Cherbourg that’s my home: celebrating landscape through song
- Creating rural attractions
- Festivals
- Queer pleasure: masculinity, male homosexuality and public space
- Railway refreshment rooms
- Regional cinema
- Schoolies week: a festival of misrule
- The sporting landscape
- Visiting the Great Barrier Reef
By:
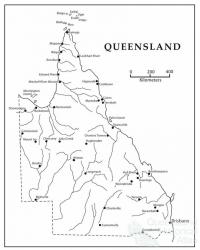
Gordon Briscoe Queensland possesses two Indigenous groups: Australian Aborigines and Torres Strait Islanders. Archaeologists have placed Aboriginal occupation at about 36 to 55 thousand years BP (before present) and Torres Strait Islander occupation in the last 3000 years BP. In ‘precontact times’ these two peoples kept healthy through traditional migration, hunting activity, good diet, plenty of cultural exercise and rest. Europeans, possibly as early as 1522, touched the east and west of the continent and Dutchman William Janzoon explored the western Cape York in 1606, 50 years before the Englishman William Dampier saw the western coast. Most Europeans saw neither good in the land nor the people. James Cook and Arthur Phillip reported Aborigines in good physical health in both 1770 and 1788 respectively.
The health, fitness and wellbeing of Queensland’s two Indigenous populations rested on the maintenance of their traditional activities, and food, as well as the slowness of the British establishing a penal garrison in 1823, together with expansion of the British population into the Brisbane valley during the 1840s. Accelerating British expansion westward and northwards from 1850 to 1900 overlaid plummeting Aboriginal medical and health conditions.
Deteriorating conditions
Pastoral conditions on the mainland affected food, cultural activities and freshwater sources. The effect of traditional migration on Indigenous Peoples' central feature of maintaining good health, and wellbeing, was immediate. Competition with the British for land, food and water saw the development of colonial programs to centralise Aboriginal populations on the mainland onto feeding and medical depots. By the 1850s Aboriginal resistance to British expansion saw the introduction and reliance on ‘native police forces’. Punitive expeditions created massacres across the colony by the 1880s, and known Aboriginal populations dwindled from more than 200,000 in 1839 to 15,000 in 1897, and at the same time, British populations increased. Reports on the deteriorating conditions of life of Aborigines on the mainland including increasing vicious attacks by native police, and pastoralists’ killings of Aborigines, forced the colonial regime to disband the native police and increase protection arrangements for Aborigines. Archibald Meston and Dr Walter Roth were crucial supporters for both protection legislation and Protectors of Aborigines in the last decade of the nineteenth and first decade of the twentieth century.
In 1901 Federation occurred where Queensland shared economic, political and cultural legislative powers with the Commonwealth. Control of hospitals, medical services, ambulatory health services and race relations remained with Queensland who repatriated South Sea Island slaves in 1907. Immigration was shared in the interim but control over quarantine was held by the Commonwealth. Plantation labour and infectious diseases began to affect Aborigines on the mainland and the Torres Strait, together with remaining South Sea Islanders. Infections like leprosy, tuberculosis, hookworm, influenza and mental and sexually transmitted diseases began circulating between white Queenslanders and Indigenous rural populations. Missionaries cared for sick Indigenous groups during periodic epidemics in outlying regions and contract nurses and doctors cared for Aborigines on Government reserves or ration depots.
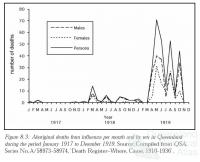
Epidemics
By the end of World War I, most bush hunter and gatherers on the mainland were either in contact with missions or on cattle properties as surplus labor and on government reserves. There were also large numbers of Aborigines either on the Palm Island’s government penal or medical establishments for treatment of tuberculosis and leprosy. Some research of Aboriginal health was carried out by the Commonwealth and mortality records were collected by the Queensland Government while primary health nurse-based-clinics were presented on government reserves.
Fringe-camp conditions were exacerbating Aboriginal health profiles due not only to scarce government presence in the Cape and Gulf regions but also due to poor living conditions on government depots before World War II. Once events like the 1918-19 Influenza Pandemic came and went. This made arresting epidemics of measles, leprosy, tuberculosis and periodic influenza an almost impossible task - both to bring the sick to hospitals and to carry out follow-up treatment. Added to these difficulties was the dual problem of state ‘user pays primary health’ and overlapping commonwealth public health systems. Between the Wars, State/Commonwealth and international Hookworm treatment made cumbersome programs more difficult. The living conditions of Aborigines were made harder too, with the absence of knowledge of treating viruses such as tuberculosis, leprosy, measles and influenza. These all came under control after World War II with antibiotics.
Torres Strait
In the Torres Strait the Thursday Island Hospital served the whole Torres Strait region, a position neither pleasing the Indigenous populations of the mainland nor the Islands. In the period from 1945 to the present, greater periodic medical, political and social change bought greater primary and public health changes.
Medical, social and political change
The greatest impediment to Aboriginal health was not just that Indigenous peoples were caught in a social, economic and political transition but that their differences were exacerbated by both separate legislations that managed political change; and divided state and federal governance structures. In 1897 the Aboriginal ‘protection’ from colonial ravages came under British legislation called the Aboriginals Protection and Restriction of Sale of Opium Act, 1897. This legislation was without a political movement as its critique and as a result subjugated modern Indigenous societies. In the period from 1949 to the 1960s, Queensland could boast better conditions of life than most Aboriginal communities around Australia. However, the mining boom of the 1970s and 1980s in the Cape region, arrested some economic and social justice change. Change did come during the 1970s-80s, however, as the Commonwealth brought a fresh medical and bureaucratic perspective. Aboriginal health and welfare policies introduced a more equal treatment. Today, while diseases like diabetes, obesity and the effects of alcohol take the place of disappearing ‘protection and assimilation’ policies, lifestyle diseases are replacing both abnormally high Indigenous infant mortality and a plummeting life expectancy. Following close behind these changes in Indigenous health is greater consciousness by all governments to public health.
References and Further reading (Note):
Gordon Briscoe, Counting, health and identity: a history of Aboriginal health and demography in Western Australia and Queensland, 1900-1940, Canberra, Aboriginal Studies Press, AIATSIS, 2003
References and Further reading (Note):
Gordon Briscoe, Aborigines and the Spanish influenza pandemic of 1918-1919, Canberra, AIATSIS, 1996
References and Further reading (Note):
Hazel M. Smith and Ellen H. Biddle, Look forward, not back: Aborigines in metropolitan Brisbane, 1965-1966, Canberra, ANU Press, 1975
References and Further reading (Note):
Basil L. Hetzel, Malcolm Dobbin, Lorna Lippmann, Elizabeth Eggleston, (eds), Better health for Aborigines?, St Lucia, University of Queensland Press, 1974
References and Further reading (Note):
H.C. Coombs, Kulinma: listening to Aboriginal Australians (and Torres Strait Islanders), Canberra, ANU Press, 1978
References and Further reading (Note):
Peter M. Moodie, Aboriginal health, Canberra, ANU Press, 1973
References and Further reading (Note):
Neil Thompson (ed), The health of Indigenous Australians, South Melbourne, Oxford University Press, 2003
Keywords:
Aboriginals, Aborigines, diet, disease, health, hospitals, Indigenous, living conditions, massacre, medicine, population, public health, Torres Strait Islanders